- Licensed & Approved Agency in Multiple States
- (888) 901-4870
- (404) 996-0045

Mutual of Omaha Medicare Supplement Insurance
July 14, 2021
Annual Medicare Enrollment
September 22, 2021What is the Medicare Part B Give Back Benefit?
We’ve all seen the commercials with Joe Namath, and now Jimmie Walker “Dyn-O-Mite!”… regarding your Medicare coverage options and the Medicare Part B give back benefit. To learn more about what is covered under Medicare Part B, click → Medicare Part B Benefits.
The Medicare Part B give back benefit is a way to save money on your Medicare Part B monthly premium ($170.10 standard amount per month for 2022). This premium is paid directly to Medicare each month either by you or drafted out of your Social Security benefits if you’re collecting. Here are a few facts about accessing these savings.
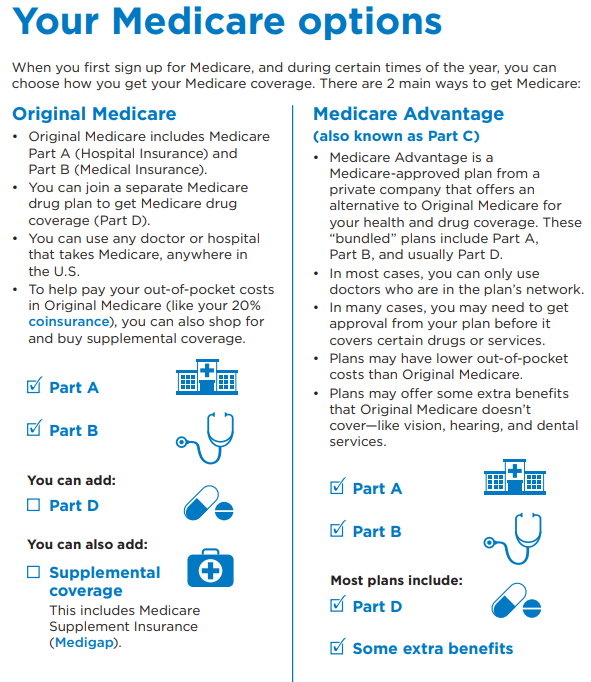
If you’re looking to maximize your savings while on Medicare, you may be wondering, what is the Medicare Part B give back benefit? This benefit is not an official Medicare program but another name for a Medicare Part B premium reduction, included in some Medicare Advantage “Part C” plans. Whether you receive this reduction depends on the conditions of the plan you choose and a few other factors. Read on for three facts about this benefit.
You Need to Be Enrolled in a Medicare Advantage Plan (also known as Part C)
According to the official U.S. government website for Medicare, some Medicare Advantage plans cover part or all of your Medicare Part B monthly premium. To enroll in a Medicare Advantage plan, you need to be enrolled in or eligible for both Medicare Part A and Medicare Part B.
The only way to get the Medicare Part B give back benefit is to enroll in a Medicare Advantage plan in your county. Not all Medicare Advantage plans will offer it.
Location Is Key
According to the official U.S. government website for Medicare, the Medicare Advantage plans available to you differ according to your zip code. This is because Medicare Advantage plans are offered by private insurance companies (Humana, Aetna, Wellcare, Anthem, etc.) who determine the specific service areas of their plans.
Certain states or regions may offer Medicare Advantage plans that cover some or all of Part B premiums, while others may not. Unfortunately, if you live in an area that does not provide such a plan, you can’t take advantage of this benefit.
Your Plan Could Change Its Premiums
The official U.S. government website for Medicare reports that, even though private insurers must follow Medicare’s rules for coverage in their Medicare Advantage plans, they each individually set the fees they charge for premiums, deductibles, and services.
Each private insurer offering Medicare Advantage plans can alter the fees associated with their plans once a year. This means that your plan could offer the Medicare Part B give back benefit one year, which can change for the upcoming plan year.
These changes can only take place once a year, on January 1. Be sure to review any alterations to your plan after this date.
I’m more than happy to show you all of your Medicare plan options available in your area to find what’s best for you. 🙂
Are you interested in learning more about Medicare, Medigap, and Medicare Advantage plans available in your area?
If so, schedule a call with me here → Schedule Call with Chad.
You can also call (888) 901-4870 to set up a phone call with me.